Types of Knee Surgery for Arthritis Treatment
There are several different types of surgery offered to treat knee arthritis. Which surgery, if any, is recommended will depend on several factors, such as the patient’s age, anatomy, general health, lifestyle, and personal preferences, as well as the surgeon’s experience and preferences.
Total Knee Replacement Surgery (Total Knee Arthroplasty)
Total knee replacement surgery involves cutting the damaged ends of the tibia (shin bone) and femur (thighbone) and capping both with prostheses. Read Undergoing Total Knee Replacement for Knee Arthritis
Patients with moderate to severe knee arthritis who have exhausted non-surgical treatment options might consider replacing the entire knee joint. The surgery involves cutting the arthritically damaged ends of the tibia (shin bone) and femur (thighbone) and capping both with prostheses (like capping teeth).
The two prosthetic pieces are made of either metal or a durable plastic called polyethylene. These new surfaces move smoothly against one another, creating a functional knee joint. Partial recovery typically takes 4 to 6 weeks1 and full recovery may take a few months to an entire year.
Total knee replacement surgery provides most patients with pain relief and improved knee joint function. However, a replacement knee is not as strong and durable as a healthy knee, and patients are strongly advised not to engage in high-impact activities (such as jogging) that may speed up the wear-and-tear of the new joint.
See Minimally Invasive Knee Replacement Surgery
Partial Knee Replacement Surgery (Unicompartmental Knee Arthroplasty)
Partial knee replacement, often called unicompartmental knee replacement, involves replacing only one of the knee’s three “compartments”:
- The medial compartment refers to the inner knee (where a person’s knees touch when the legs are together).
- The lateral compartment refers to the outer knee.
- The patellofemoral compartment is at the front of the knee, where the patella (kneecap) meets the femur (thighbone).
Partial knee replacement surgery treats the arthritically damaged compartment of the knee joint (typically the lateral or medial compartment) while preserving healthy areas. This surgery is appropriate for only a small number of people, and patients may be ineligible if their knees are not well aligned (e.g. bowlegged or knock-kneed), have severe knee stiffness, have ligament damage, or if they suffer from inflammatory arthritis, such as rheumatoid arthritis.
Compared to total knee replacement, partial knee replacement is less invasive, so it is usually less painful and requires less recovery time. However, partial knee replacement is not as reliable as total knee replacement for alleviating pain.
See Managing the Pain of Joint Replacement
Knee Osteotomy (Tibial Osteotomy or Femoral Osteotomy)
During a knee osteotomy, a small wedge of natural bone graft or artificial bone material is inserted in the bone to realign the joint. Read Knee Osteotomy Surgery
This surgery is appropriate for a limited number of younger (under age 60 or so), physically active people whose poor knee alignment has caused a great deal of wear-and-tear on just one side of the knee joint, a condition called unilateral knee arthritis or asymmetrical knee arthritis.
During knee osteotomy the surgeon cuts into the femur (thigh bone) or tibia (shin bone) and either:
- Removes a small wedge of bone, or
- Adds a small wedge of natural bone graft or artificial bone material.
Knee osteotomy re-aligns the joint to shift more pressure onto the “good” side of the knee joint and reduce wear and tear on the bad side. The goal is to reduce pain and perhaps slow down the progression of knee osteoarthritis. A successful knee osteotomy surgery can postpone the need for total knee replacement surgery up to 10 years.2
Unlike after total knee replacement, recovered knee osteotomy patients may participate in high-impact sports.3 This is a major surgery with potential risks and complications, and patients must be committed to extensive post-surgical physical therapy. A full recovery may take months or even an entire year.4
Read more about the procedure, risks, and recovery timeline for: Knee Osteotomy Surgery
Knee Arthroscopy
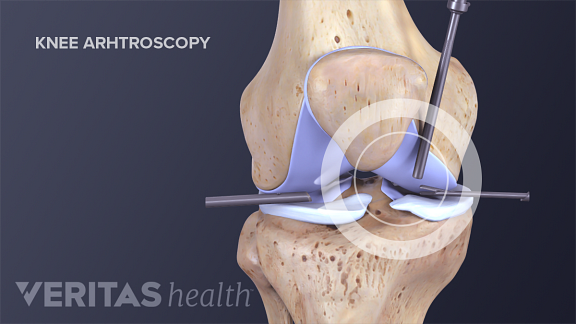
In arthroscopic surgery, the surgeon inserts a video camera and surgical tools through small incisions and can make an assessment of arthritic joint degeneration.
Arthroscopic surgery requires only small incisions through which the surgeon inserts a very small video camera and surgical tools. During knee arthroscopy, a surgeon can make an assessment of joint degeneration due to arthritis.
The surgeon can also perform knee debridement and lavage, which includes the following process:
- Remove loose pieces of cartilage or bone (loose osteophytes) suspected of causing irritation
- Trim or smooth out cartilage that has grown irregular and bumpy
- Remove inflamed synovial tissue
- Flush the joint with a saline solution, a process called lavage, to clean out materials known to cause irritation and swelling
Experts’ opinions differ on whether knee arthroscopy is a worthwhile treatment option for knee osteoarthritis. Some experts point to clinical studies that suggest knee arthroscopy does not provide benefit to knee osteoarthritis patients.5,6 Others reason that because knee arthroscopy is less invasive and carries fewer risks it is worth trying before embarking on a more invasive surgery, such as total knee arthroplasty.7 (Most experts do agree arthroscopy is useful for treating other knee problems, such as repairing meniscal tears.) Knee arthroscopy is an outpatient procedure, but it is still surgery and it can take 6 to 8 weeks for the joint to fully recover.
Cartilage Repair and Cartilage Restoration
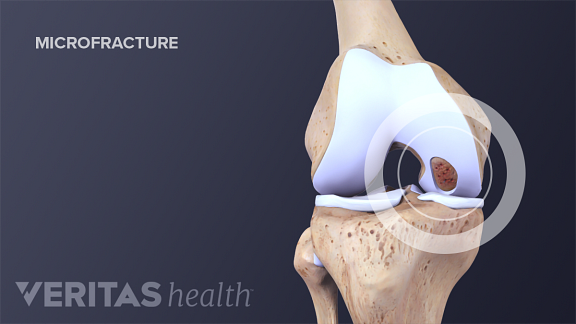
One way to stimulate cartilage growth is by making precise microfractures in the surrounding bone.
This procedure is called bone marrow stimulation.
Once damaged, cartilage does not heal well. Even if the joint is able to grow new cartilage, it tends to be rough and bumpy and therefore less able to facilitate smooth movement at the joint. There are a handful of surgeries that attempt to repair or encourage the growth of healthy cartilage:
- Bone marrow stimulation, which stimulates cartilage growth by making precise microfractures in the surrounding bone
- Osteochondral transplantation techniques (OATS), also referred to as “mosaicplasty,” which involves transplanting cartilage from one site to another
- Autologous chondrocyte implantation (ACI), which requires two surgeries. In the first, cartilage cells are harvested and then grown in a laboratory for several weeks. During the second surgery the cartilage cells are re-implanted.
These procedures may be appropriate for patients who have a relatively small and very isolated area of articular cartilage damage. Typically, these patients are younger and have damaged their cartilage through trauma (e.g. a sports injury) rather than over years of gradual wear and tear. Therefore, these surgeries are usually more appropriate for people trying to slow or prevent severe arthritis rather than alleviate it.
This article focuses on the most common types of knee surgery for arthritis. New types of surgery, less invasive surgical techniques, and new implant designs and materials are the subjects of ongoing research.
People suffering from knee arthritis should make a concerted effort to alleviate symptoms with non-surgical treatments. If non-surgical treatments do not provide satisfactory pain relief and improved knee function, then an orthopedic surgeon who specializes in knee surgery can determine whether surgery is an appropriate option.
Learn more about how doctors such as orthopedic surgeons treat arthritis in Arthritis Treatment Specialists
In addition to recommending a specific surgery or set of surgeries, the surgeon will explain the surgery’s potential benefits, expected recovery period, and potential risks and side effects, as well as alternatives to the surgery. Once fully informed, the patient can decide whether or not to have the surgery.
Disclaimer: This article has been taken from https://www.arthritis-health.com/ as it is. Click here to read the original article.



 Knee Osteoarthritis Video
Knee Osteoarthritis Video